| Continuous
HAART Associated with Elevated Risk of Bone Loss in SMART Treatment Interruption
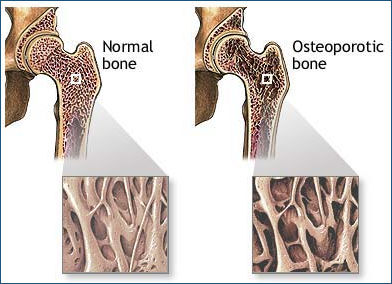
Trial Evidence has accumulated over the past several years showing that antiretroviral treatment interruption guided by CD4 cell count is a risky strategy that can lead to a higher risk of both AIDS-defining opportunistic illnesses and serious conditions such as cardiovascular disease that are not traditionally considered HIV-related, but may be due to inflammation and other abnormalities associated with ongoing viral replication. Researchers initially explored structured treatment interruption in an effort to spare patients some of the side effects, inconvenience, and costs of life-long therapy. But most studies to date have demonstrated few such benefits, especially given the development of more tolerable and easier to use drugs. The latest analysis from the large SMART trial, however, indicates that continuous HAART may increase the risk of bone loss (osteopenia, or the more serious osteoporosis). Data were presented this week in a late-breaking poster at the 48th International Conference on Antimicrobial Agents and Chemotherapy (ICAAC) this week in Washington, DC.
Research
looking at bone mineral density (BMD) in people with HIV has produced conflicting
results. Several studies have shown that HIV positive people have lower BMD compared
with the general population, but it is not clear whether this is related to HIV
infection itself, antiretroviral therapy, an accelerated aging process, or other
unknown factors. Hip and spine BMD were measured annually using dual-energy x-ray absorptiometry (DEXA), and trabecular BMD of the spine was assessed using quantitative computed tomography (CT). The investigators used longitudinal models to compare BMD changes in the 2 arms, and assessed the incidence of reported fractures in the study as a whole. Further, they evaluated associations between BMD decline and cumulative antiretroviral drug use in the continuous therapy arm. At baseline, 12% of the patients had osteoporosis, median t-scores (a standard measure of bone density) were -0.5 for the femur, -0.9 for the spine by CT, and -0.7 for the spine by DEXA. Participants were followed for a mean of 2.4 years. Results
Based on the results of this analysis, the researchers concluded that, "Continuous antiretroviral therapy is associated with decline in BMD and possibly more fractures relative to intermittent, CD4-guided antiretroviral therapy." Given the now-obvious detrimental effects of treatment interruption, however, they emphasized that "Intermittent antiretroviral therapy is not recommended due to increased risk of AIDS and death observed in the SMART study." Univ. of Minnesota, Minneapolis, MN; St. Vincent's Hosp. and Univ. of NSW, Sydney, Australia. 10/31/08 Reference |
The
material posted on HIV and Hepatitis.com about ICAAC 2008 and IDSA 2008 is not
approved by nor is it a part of ICAAC 2008 or IDSA 2008. |
![]()